
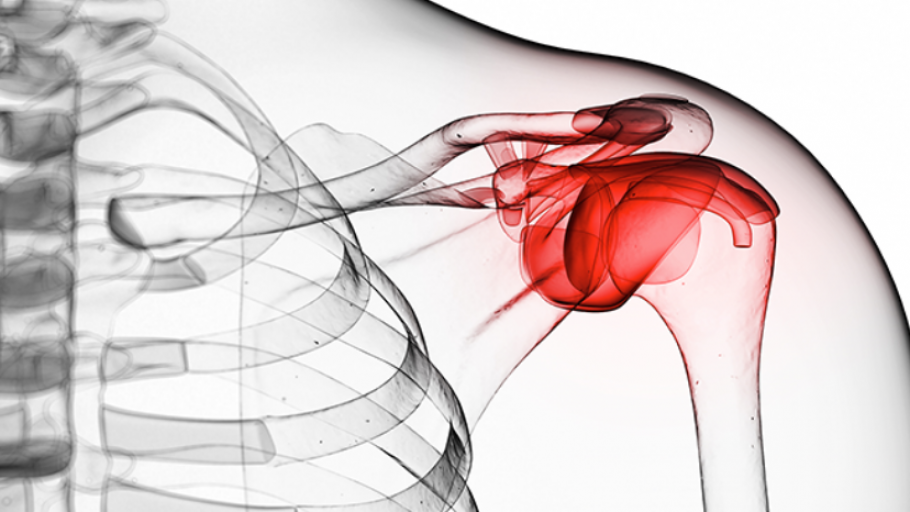
Frozen Shoulder – Adhesive Capsulitis
Frozen shoulder, also known as adhesive capsulitis, is a condition that causes stiffness, pain, and limited mobility in the shoulder joint. It typically develops gradually and can significantly impact daily activities. It often starts after a shoulder insult such as shoulder surgery, joint damage or rotator cuff tear, each where the shoulder is often immobile for a period of time.
The actual tissue damage is still not well understood. The joint connective tissue seems to go through an inflammatory phase, then a stiffening phase, before starting to recover by itself. There is growing evidence it could be some type of autoimmune condition.
Symptoms
Stage 1: Freezing Phase
- Gradual onset of shoulder pain, which worsens over time.
- Stiffness begins, limiting shoulder movement in most directions.
- Pain is often worse at night, affecting sleep quality.
Stage 2: Frozen Phase
- Severe stiffness with marked reduction in mobility.
- Pain may decrease, but the shoulder remains immobile.
- Difficulty performing everyday activities, such as dressing or reaching.
Stage 3: Thawing Phase
- Gradual improvement in mobility as stiffness subsides.
- Pain diminishes significantly during this phase.
- Full recovery can take months or even years.
Causes of Frozen Shoulder
The exact cause of frozen shoulder is not always clear, but several factors can contribute to its development:
- Injury or trauma: Shoulder injuries, such as fractures or rotator cuff tears, can lead to immobilisation and potentially cause frozen shoulder.
- Prolonged immobility: Extended periods of inactivity, such as post-surgery or resting the shoulder after an injury, can increase risk.
- Underlying health conditions: Conditions like diabetes, thyroid disorders, and cardiovascular diseases are associated with higher likelihood of frozen shoulder.
- Age and gender: Typically affects individuals aged 40–60 and is more common in women.
- Inflammation: Chronic inflammation in the shoulder joint can contribute to stiffness and pain.
- Stress: There is growing evidence that a stressful lifestyle can contribute to developing frozen shoulder


Treatment Options for Frozen Shoulder
This is where Clinic 88 comes in! We pride ourselves as being Canberra’s most skillful manual therapists.
Manual therapy can be very effective in managing frozen shoulder, alleviating pain and improving mobility. It fast tracks your progress through the three phases – especially phase 3 where the biggest changes with treatment occur.
Don’t be fooled into believing there is a magic cure for frozen shoulder. There isn’t. Time is needed for the shoulder damage to repair. Treatment often helps reduce pain and increase mobility but time is still necessary for full recovery.
You may start to get rapid changes with manual therapy in the ‘thawing’ phase of frozen shoulder. This is when the shoulder is healing itself and is often more responsive to treatment.
Joint Mobilisation
- Gentle techniques to improve the range of motion in the shoulder joint.
- Focuses on reducing stiffness and enhancing flexibility.
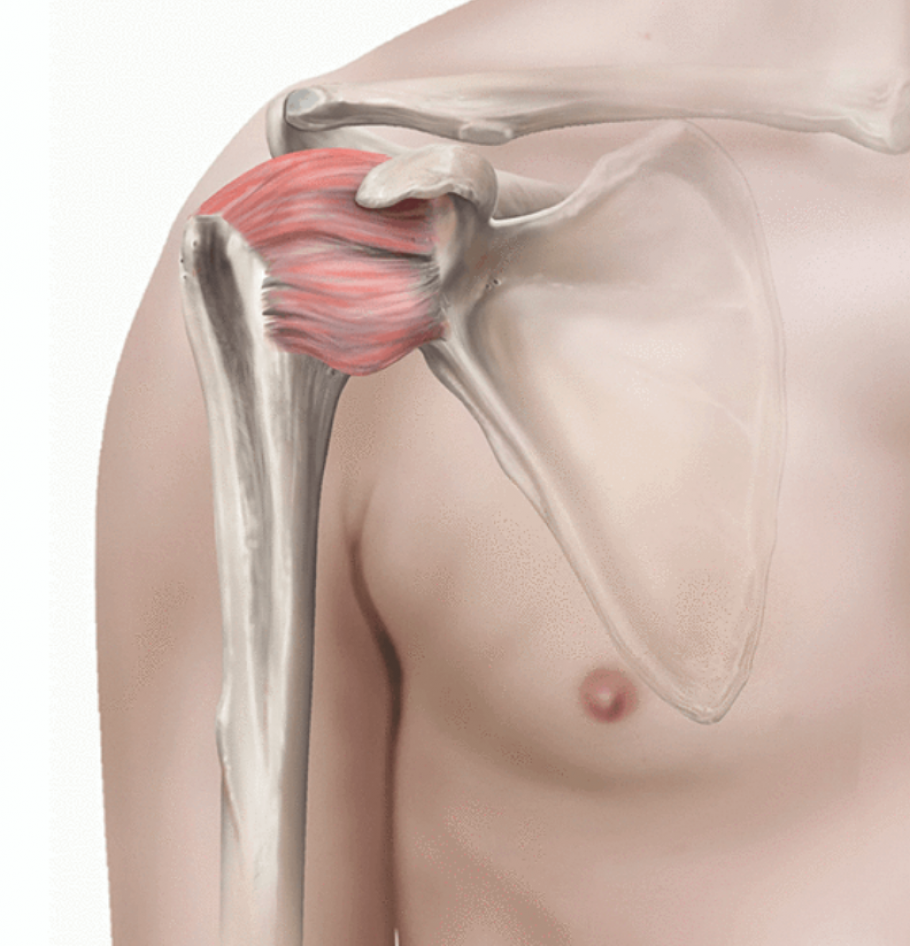
Soft Tissue Massage
- This focuses on the rotator cuff (four muscles that stabilise and move the shoulder joint). Some or all of these muscles are often a major component of your frozen shoulder symptoms
- Focusing on areas beyond your shoulder is important to reduce any cervical (neck), scapula (shoulder blade) or thoracic spine (upper back) involvement
Stretching Exercises
- Active (moving while stretching) and passive stretches (stretching while staying still) to improve shoulder mobility.
- These are often repetitive swaying motions of the shoulder joint, while holding a weight of some type. This distracts the connective tissue of the joint, adding a stretch to this tissue, while taking it gently through a range of motion that you have lost
- These can slowly progress as your symptoms reduce
- Don’t start to aggressively or you run the risk of worsening your symptoms
Dry Needling
- Targets trigger points to release muscle tension of local muscles and referred pain that can exacerbate or mimic frozen shoulder pain
- Dry Needling often has analgesic effect
Postural Correction
- Addresses poor posture habits that may exacerbate shoulder stiffness.
- Focuses on realigning the shoulders and upper back.
Lymphatic Drainage
- Reduces swelling and enhances fluid movement around the shoulder.
- Promotes healing and reduces inflammation.
Strengthening Exercises
- Builds endurance in the shoulder and surrounding muscles. This usually begins in the ‘thawing’ phase as exercises are almost impossible during the first two phases
- Focuses on restoring functional movements.
Medical and Surgical Options
In cases where manual therapy is insufficient, medical and surgical interventions may be considered:
Medical Treatments
- Anti-inflammatory medications: Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation.
- Corticosteroid injections: Targeted injections into the shoulder joint provide relief from inflammation and pain.
- Hydrodilatation: A procedure where saline solution is injected into the shoulder joint to stretch the capsule and improve mobility.
Surgical Treatments
- Manipulation under anesthesia: The shoulder is moved through its range of motion while the patient is under anesthesia to break adhesions.
- Arthroscopic capsular release: A minimally invasive surgery where tight portions of the shoulder capsule are released to improve mobility.

Frequently Asked Questions
What is frozen shoulder?
- Frozen shoulder is a condition characterised by pain, stiffness, and limited mobility in the shoulder joint, often progressing through three distinct phases.
- The exact reason for this occuring is still not well known
- The exact damage to the shoulder joint and local muscles is still not well known
- There is growing evidence it may be an autoimmune condition
How long does frozen shoulder last?
- Frozen shoulder typically lasts between 1 and 3 years, depending on the severity and treatment approach.
Can frozen shoulder be prevented?
- Yes, maintaining regular shoulder movements, timely treatment of injuries, and addressing underlying conditions like diabetes can help prevent frozen shoulder.
Is manual therapy effective for frozen shoulder?
- Yes, manual therapy techniques such as joint mobilisation, stretching, and massage can alleviate pain and improve shoulder mobility.
How does dry needling help frozen shoulder?
- Dry needling targets muscle tension and trigger points, promoting relaxation and improving shoulder mobility.
Can posture contribute to frozen shoulder?
- Poor posture can exacerbate stiffness and pain. Addressing postural imbalances can aid in recovery.
What medical treatments are available for frozen shoulder?
- Anti-inflammatory medications, corticosteroid injections, and hydrodilatation are effective options for managing pain and inflammation.
Can Frozen Shoulder come good by itself?
- Yes. Frozen shoulder in most circumstances will come good on it’s own. However this may take 12 months to 3 years